The Magazine of the Association of Salaried Medical Specialists | ISSUE #138 | MARCH 2024 INTERVIEW MINISTER OF HEALTH DR SHANE RETI P.04 SPOTLIGHT ON ARTIFICIAL INTELLIGENCE THE IMPLICATIONS & APPLICATIONS OF AI IN NEW ZEALAND HEALTH CARE P.12–21 KENEPURU HOSPITAL & THE POSTCODE LOTTERY WHAT THE FUTURE OF PORIRUA’S AFTER HOURS ACCIDENT & MEDICAL CLINIC CAN TELL US P.22
ISSUE #138 MARCH 2024
This magazine is published by the Association of Salaried Medical Specialists and distributed by post and email to union members.
Executive Director: Sarah Dalton
Magazine Editor: Andrew Chick
Journalist: Matt Shand
Designer: Twofold
Cover Image: Sezeryadigar/iStock
The Specialist is produced with the generous support of MAS.
WANT TO KNOW MORE?
Find our latest resources and information on the ASMS website asms.org.nz or follow us on Facebook and Twitter.
Also look out for our ASMS Direct email updates.
If you have any feedback on the magazine or contribution ideas, please get in touch at asms.org.nz
PREFER TO READ THE SPECIALIST ONLINE?
We have listened to your feedback and are aware that some members prefer not to receive hard copies of the magazine.
If you want to opt out of the hard copy, just email membership@asms.org.nz and we can let you know via email when the next issue is available to read online.
ISSN (Print) 1174-9261
ISSN (Online) 2324-2787
The Specialist is printed on Forestry Stewardship Council® (FSC®) certified paper.
Proposed position for FSC logo and text. Please align to bottom of this margin.

INTERVIEW: MINISTER OF

A new year, a new health minister and a new direction for Te Whatu Ora.
PROFILE: SIR COLIN TUKUITONGA Leaving the tent
A lack of faith in the new coalition Government saw a prominent Pacific health advocate walk away from prestigious positions.
UPFRONT 02 Cutting remarks 03 Urgent consultation IN BRIEF 31 ASMS 2023 Salary Survey published 32 National Executive and Branch Officer elections 32 6,000th member qualified twice to work in New Zealand 08 Timing is everything FEATURES 12 The robot doctor will see you now? 14 DiNA – a new face of medicine 16 Being mindful of the machines 20 AI in health care (written by an AI) 22 By the numbers: Kenepuru Hospital and the postcode lottery 26 Volunteering to change 28 Prescribing a lower road toll 04 06
HEALTH SHANE
RETI Reti, steady, go
MARCH 2024 PAGE 1

CUTTING REMARKS
JULIAN VYAS, ASMS PRESIDENT
Cuts to government spending won’t make a better health system.
To meet their commitment to cut taxes, it appears the new Government is embarking on an austerity plan of sorts. This will undoubtedly reduce funding to the broader health system, but it will harm the most vulnerable in our society and, in turn, increase demand on the same services that face those funding cuts.
Finance ministers of all stripes blithely announce that savings of ‘x per cent’ can be made, followed by instructions to other ministers to actually find out how to do it. I’m not an economist, but issuing such edicts – without even knowing how they might be achieved – suggests a blinkered view that I’d expect from a recalcitrant teenager, not the people running our country.
For many years now, health system funding has not been lavish. The system’s shortcomings are multifarious. Given the long-standing failure to properly invest, it is worrying that the solution proposed for those symptoms is a treatment that will cause more of the same symptoms. This is the principal upon which homeopathy is based.
As doctors, our working day is beset with problems caused by antiquated, ill-conceived, or inadequately resourced systems. As one example, members (and colleagues in other health professions) face waiting months before we get our backpay lump sums from pay settlements. This has been blamed on payroll systems that are so outdated they are still at risk from the millennium bug.
Were this the only problem, it might be tolerable. In the context of shockingly poor workplace cultures that, in some instances, have caused serious harm to patients, a protracted failure to honour pay agreements is a sure-fire recipe for further unrest within the health workforce.
I understand that a new Pulse survey is being drafted. This seems pointless when the results of the first one have not been properly shared – let alone any necessary changes implemented.
This is my last column for The Specialist – my time as President finishes on the 31st of March. It has been an honour and a privilege to have served as your President. I am so very grateful to have been given the opportunity to do so.
Over the last few years, I think that ASMS has become considerably stronger and more mature as an industrial organisation. We are valued as an opinion leader on the subject of New Zealand’s health system; we have over 6,100 members, healthy finances and excellent governance processes; and we are planning further investment in our infrastructure to provide better support for members – including a better understanding of local workplace agreements across the country.
Last year in particular, Annual Conference’s decision to add two Māori members to the National Executive, and our first national strike, show our maturation as a union. I am very grateful to members for supporting both of these.
I’m pleased to announce that Katie Ben will be your new President, starting on the 1st of April 2024, and Sylvia Boys will be your Vice President. Apart from the fact that they are very able occupants of these roles, I’m also really pleased that Katie is ASMS’ first female President. Another step forward.
Finally, I must give my deepest thanks to Andrew Ewens as Vice President, and to the whole of the National Executive for their hard work throughout the last three years. In particular, I think it is also worth acknowledging outgoing executive members Julian Fuller and Seton Henderson, who between them have given 24 years’ service on our Executive.
Likewise, I’m also extremely indebted to Sarah and everyone who works for ASMS – for all they have done to support me in the last three years, and, much more importantly, all that they continue to do for all our members.
Kia kaha
It has been an honour and a privilege to have served as your President. I am so very grateful to have been given the opportunity to do so.”
– JULIAN VYAS
PAGE 2 THE SPECIALIST
URGENT CONSULTATION
SARAH DALTON, EXECUTIVE DIRECTOR

Is Te Whatu Ora in a position to hear our concerns? And how can you ensure ASMS best listens to yours?
Te Whatu Ora is currently trying to decide what to do about after-hours medical care around the country. We haven’t yet been consulted or asked to meetings, but we know it’s another item on their long list of things to do.
For the people of Porirua and the Kāpiti Coast, after-hours care is provided at Kenepuru Hospital. It’s a patched-together model: a mix of local GPs, contractors and employees. While some good things are happening – and the staff there are great – it’s a service subject to significant failure to invest over a long period of time.
Under Te Whatu Ora, the service sits uncomfortably between the ‘Commissioning’ and ‘Hospital and Specialist Services’ arms – with all the complications that entails.
Te Whatu Ora is toying with replacing face-to-face care after 10 pm with telehealth. I find it incredible that telehealth could be the preferred afterhours care platform for a high-needs urban population of over 110,000 people. This cannot be the way forward in a system that is supposed to improve people’s access to care.
It leads me to wonder why it’s so difficult to get things done in our newly joined-up system? Is it joined up yet? And at what point will we be able to give it a vote of confidence?
Money is still tight. That’s a soft way to say that health investment is unlikely to increase any time soon. The shopping list is still larger than the bank balance, and just keeping the lights on continues to be a challenge. Only today I heard of a facility where people are expected to work alongside black mould.
Meanwhile, the next iteration of the Te Whatu Ora Pulse survey has been announced. While the last thing you need in your working day is another survey, I encourage you to respond to this one in blunt and honest terms so whomever reads your responses gets the benefit of your lived experience.
I know that everything out there is not gloomy – and clinicians continue to make sure people get the care they need. But as I meet with members at the
It leads me to wonder why it’s so difficult to get things done in our newly joined-up system.”
– SARAH DALTON
first round of JCC meetings, the overall picture is one of discouragement, epic understaffing and flailing leadership.
This is why we’ll be campaigning for sustainable staffing, and improved models of provision, in places like Kenepuru. It’s also why we’ll be taking more compliance actions over the coming months.
Meanwhile, it’s election time for the ASMS Executive. I want to thank our outgoing executive for their last three years of service to ASMS. They have worked incredibly hard to advance your interests. I’m not sure any other exec has been required to bargain collective agreements each and every year of their term at the same time as an international pandemic, and while a new health system is established. They have been staunch throughout, and never stepped back from the considerable demands made of them.
I especially want to acknowledge Julian Vyas’ work as your President. It has been fantastic working alongside him over the past three years. I also want to acknowledge Carmel for sharing Julian with us. I know there have been occasions when ASMS has taken priority. I hope you enjoy seeing more of him after April!
I also want to congratulate Katie Ben, who has stood unopposed and will be ASMS’ next President. It will be another year bargaining for a new Te Whatu Ora collective agreement – and there are plenty of other challenges too. She will be setting out her agenda in the June issue.
As to the other members of the new Executive, I hope as many of you as possible will take a few minutes to read about the candidates and send in your votes when voting papers are emailed to you – and encourage your colleagues to do the same.
MARCH 2024 PAGE 3
“They [Te Whatu Ora] have taken the message from me that frontline is my priority. That’s where I want to see resources.”
– DR SHANE RETI
RETI, STEADY, GO
MATT SHAND, JOURNALIST
A new year, a new health minister and a new direction for Te Whatu Ora.
Doctor and newly appointed Minister of Health Shane Reti minces no words when it comes to labelling the state of the health care system as a crisis.
“I have no issues calling it what it is,” he said.
“They [Labour] did not want to touch those six letters. I have no issue calling it that. One, it reflects the urgency that you give to where we are. Secondly, it shows some degree of understanding. To not call it what it is, is tone deaf. Almost every meeting I went to where the previous minister was present, the first question from the floor was ‘Is it a crisis or not?’”
Reti says the health care system will no longer be in crisis when everyone has “timely access to quality health care”. To realise this goal, he plans to take the health care system, and Te Whatu Ora, in a new direction with less centralisation and with local decision making put back into patient care.
“When you pass decision making [locally] we pass up accountability,” he said. “That’s a desirable thing. That gives accountability to a region.”
This decentralisation will come at a cost. The major cost will be the disestablishment of Te Aka Whai Ora and its Māori-focused health lens. Reti has no doubt it will be scrapped in favour of other options.
“The previous [Labour] Minister of Health said the single biggest hurdle to the health system was quote, ‘failure to embody the Treaty of Waitangi’.
I disagree,” he said.
“The single biggest hurdle to our health care system is workforce, workforce, workforce.
“So, fundamentally, we have a difference of approach. The philosophy that centralisation of the health system, and that Wellington knows best, doesn’t work for me or this Government.
“The centralisation of all Māori health contracts to Wellington is the opposite of the direction I want to travel in. I want to have decision-making close to the home, and the tiers of decision making between the patient and system were just too many.
“I will disestablish it, but I will empower local communities to have more of a say in their own health pathway. We believe services should be close to the home and close to the hapū and should have local decision making and accountability. So, it is quite different thinking around the structure of a system.”
He says the detail of what greater local decision making and accountability are, is still being worked out, but at this stage it will not include the return of elected officials like the previous DHB model.
“Will I reintroduce 20 DHBs? The answer is no,” he says.
“But will I have regionality? The answer is yes. What does that look like? We’re still working that through, but I have said that it won’t happen tomorrow, next week, next month or, indeed, this year.
“We’ve said we wouldn’t undertake major structural change on day one. The sector is tired. They are exhausted. They’ve got change fatigue. My colleagues said they would fight me if I did major structural change – we are in a settling-in phase to conduct inventory. What projects are underway and what are the human and capital resources and the policies required?
“Part of the principle of decentralisation is bringing the patient voice closer to you.”
While change will require infrastructure spending, Reti is quick to point out this year’s Budget will not accommodate everything.
“Everyone is not going to get their wish lists this coming Budget,” he said.
“These are the fiscal cliffs we need to deal with, which means in the Budget some things will pause. It is a pause. It is not a stop.”
Reti says the changes that do occur are geared towards bringing patients closer to their public health system.
“Part of the thinking of moving from a centralised model to a decentralised model is you get more of the patient voice, and the community voice, whether we do that through elected positions or through advisory groups,” he said.
“It’s been a discussion for many years that the health system should have clinical leadership. I’m a big supporter of clinical leadership and, if you look at the direction of travel across the portfolios, it is about more frontline and reducing the non-critical back office. For clinical people that means more people at the coal face.”
Last year saw a strong message from senior doctors about the need for better workforce pay rates, working conditions and commitment to recruitment and retention during the senior doctor strikes.
Reti says the strikes sent a strong signal throughout the health sector and he has “taken note” of the sentiment.

INTERVIEW PAGE 4 THE SPECIALIST
“Our senior colleagues are now feeling powerless that they need to take these actions,” he said.
“It was a real moment. I understand and respect the ability to peacefully agitate for terms and conditions and took note of those actions last year.
“They made the decisions they made at the time for the issues that were important for them.”
Asked if any direction has been given to Te Whatu Ora as pay negotiations will continue this year, he said the issue is operational, but a direction has been given.
“They [Te Whatu Ora] have taken the message from me that frontline is my priority,” he said. “That’s where I want to see resources.”
The next 12 months will see a lot of direction change, with Reti saying the general, umbrella statement is all about getting people timely access to health care.
“We need to prevent people getting ill and, when they get ill, we need to help them get better,” he said.
“We will focus on the high priority things, of course, like cancer and mental health, and the mechanisms we have to get there will be severalfold, including workforce, targets and greater infrastructure.”
Asked about Te Whatu Ora directly and if it has been successful so far, Reti says its formation has been rushed and pulled in several directions from previous leadership.
“It’s been a hard piece of work to bring together one of the largest public entities in the middle of a pandemic,” he said.
“Workforce has been an issue around the world from Australia, Canada and the UK, but none of them undertook major structural changes to health care in the middle of a pandemic.
“New Zealand has struggled with that rushed and hurried transition. There are good things with centralisation, and I am not against it. National immunisation programmes for instance. You should not be able to drive across a boundary and have a different immunisation procedure.
“But the implementation [of Te Whatu Ora] has struggled, as the clinical performance metrics quarter on quarter are showing. There have been some small, early benefits to the formation of Health New Zealand, but it was a hard task and they have not been given a clear mandate.”
Reti says he wants to place clear mandates and ensure accountability is held for decision makers within the health care sector.
“We’ll be holding people to account. From individuals to aggregated regional entities all the way through the national bodies and to myself in my office.”

Our senior colleagues are now feeling powerless that they need to take these [strike] actions.”
– MINISTER OF HEALTH SHANE
RETI MARCH 2024 PAGE 5
“There are a significant proportion of us working in public health that think the disestablishment of Te Aka Whai Ora is premature and ill advised.”
– SIR COLIN TUKUITONGA

LEAVING THE TENT
A lack of faith in the new coalition Government saw a prominent Pacific health advocate walk away from prestigious positions.
Sir Colin Tukuitonga says doctors have a responsibility to speak up against policies that produce worse health outcomes for New Zealand.
PROFILE
PAGE 6 THE SPECIALIST
Walking away from prestigious roles sent a strong message that Sir Colin Tukuitonga is no hypocrite when it comes to public health, particularly public health that affects Māori and Pacific peoples.
“I am not going to be an apologist for the Government,” Sir Colin Tukuitonga says.
“I will not try to defend the Government’s repeal of smoke-free legislation. It goes to the core of my being, and I find the repeal deeply offensive. You’ve got to take a stand where it matters.”
Tukuitonga leaves a string of empty chairs in his wake that will be difficult to fill. He has vacated seats at the Health Quality & Safety Commission, the Public Health Advisory Committee, the chair of the Smokefree 2025 Pacific Assurance Group and the chair of Te Whatu Ora’s Pacific Senate.
“I’ve lost a lot of friends,” he says. “People said I should have boxed on and remained in the tent, but you have to do what you believe in.
“I don’t regret whatever I said about my lack of confidence in the new administration. Reneging on the smokefree legislation is appalling. They’re saying they want more smokers so they can have more revenue to fund a tax cut. It is just immoral.
“Minister of Health Shane Reti has been distant on the smokefree repeal. It is interesting that he has passed the chain to the New Zealand First person [Casey Costello]. I imagine Reti, being a doctor, never imagined he would have agreed to this. But I guess he has to support the decisions of the group.”
The repeal will mean measures including the removal of nicotine from cigarettes and the start of the ‘smoke-free generation’ won’t take place. Since the decision was announced there have been protests at Parliament and significant discontent.
Tukuitonga says doctors need to leverage their influence to ensure public health matters are not lost in the ether.
“Doctors are in a position to better what goes on in society,” he says.
“There is a responsibility to advocate for patients and correct things that lead to poor health outcomes.
“A friend of mine is a Pacific paediatrician, and she says, if you are a Pacific doctor, it is not enough to be treating patients. You must speak up and speak out on the things that lead to poor health in Pacific children and their families.
“Like academics, there is a mandate to speak up and be critics – constructive critics – and contribute to public discourse.”
Of further concern to Tukuitonga are the position statements made about New Zealand’s willingness to participate in WHO International Health Regulations. As part of the National Party’s coalition agreement with New Zealand
First, the Government urgently issued a reservation letter to the WHO, stating it would not sign up for amendments to WHO regulations.
“This emerging issue of New Zealand not wanting to participate and contribute to the revision of the International Health Regulations –it’s unheard of,” says Tukuitonga.
“New Zealand is opting out of the planned International Health Regulations amendments that have been negotiated by everyone, including us.
“My understanding is it is fuelled by conspiracy theories that think Bill Gates and the WHO have a massive plan to take over countries and weird stuff.
“To combat pandemics, we all need to be paddling in the same direction. The smaller islands of the Pacific look to us – what we do is important to them, and they follow our models.”
With inequities already present in the health care system, Tukuitonga could no longer stand by and be part of, even by proxy, supporting measures that reduce equity by cutting services.
Tukuitonga says the equity issues that are baked into our public health system need to be addressed and ultimately cost everyone more in the long term. Walking away from responsibilities to Māori and Pacific peoples is not the way forward.
“Aside from the issues of workforce, inequities are a big issue with our health system,” he says.
“Trying to enforce a system that is one-size-fitsall is not going to work.
“You need interventions from Māori, you need interventions for older New Zealanders. You need interventions with the LGBTQI+ community. The sad fact is that whatever we have done over the years is not making a dent in outcomes. Māori still have the worst health outcomes, and that carries a cost to the entire country.”
As the Government has taken more measures that, in his eyes, will not improve health outcomes, the decision to resign his posts became more certain. The disestablishment of Te Aka Whai Ora was a major blow to his resolve.
“There are a significant proportion of us working in public health that think the disestablishment of it is premature and ill advised,” he said.
“There is a principle in public health that says people who are most affected by whatever threat need to drive their responses to those things. It is not just for the benefit of Māori and Pacific people that they are healthy. It makes our country healthier. The Government says they will go back to the directorate within Te Whatu Ora and the Ministry of Health, but that’s what we’ve been doing for the last 40 years and look where we have got.”
Tukuitonga says New Zealand is at a critical time in its politics, with Māori now uniting solidly against the Government as people start to stand up to the political rhetoric.
“People are going to say enough is enough,” he said.
“I’ve never seen Māori so adamant and so united behind an issue [ACT’s Treaty principles bill] and I suspect they are not going to sit and let this be the usual process.
“If they are pushed, I would not discount civil disobedience as a possibility. I’ve never been a protest person. I have tried to work within the system, but I just find, this time, I cannot agree. I think people who are in a position to speak up should not allow these things to happen. We need to ensure we do the right thing.”
I’ve never been a protest person. I have tried to work within the system, but I just find, this time, I cannot agree.”
– SIR COLIN TUKUITONGA
MARCH 2024 PAGE 7
TIMING IS EVERYTHING
ASMS members, particularly those employed by Te Whatu Ora, will remember ASMS ratified a new collective with Te Whatu Ora at the end of November last year. But many of the payments agreed in that settlement have yet to be made.
Months after collective agreement negotiations ended with Te Whatu Ora, the organisation has not completed its obligations to provide back pay for senior doctors and dentists covered by the deal.
A new collective agreement was ratified in November last year.
The previous agreement had expired in April, and before that, ASMS had first initiated bargaining in February 2023.
The deal included a 3 per cent plus $4,000 pay increase back dated to the start of the new agreement and a $3,500 lump sum payment.
The latest agreement will itself expire at the end of August this year.
In late December 2023, Te Whatu Ora produced a spreadsheet outlining the proposed dates, district by district, for the payment of lump sums and back pay. The dates ranged from December to June 2024. ASMS is not alone, with other unions having long delays to their settlements as well.
Even then, those dates appear to have been only ‘loose guidelines’. Some districts have made their payments earlier, but most appear to have the pushed the dates back further.
“This failure to pay out its contractual obligations to staff is unacceptable,” says ASMS Industrial Director Steve Hurring.
“It sends a message of complete disregard for our senior doctors. Any small amount of goodwill that was generated by reaching a settlement is quickly washed away when Te Whatu Ora can’t even deliver on what it so reluctantly agreed.
“As well as further demoralising doctors, it erodes public confidence when people see Te Whatu Ora doesn’t even have the systems to pay people efficiently.
“The Minister of Health has identified workforce as the key in fixing the health care crisis, and here we have an employer seemingly happy to provoke an already disgruntled workforce further by dragging its heels on a contractual commitment.”
“Industrial representatives are working district by district to get updates from management about when the agreed-upon lump sum payments and back pay will be paid out to staff,” Hurring said.
“We have noted this lack of compliance, and it will be front of mind in this year’s bargaining.”
Shift allowances
Alongside the salary increases, another significant component of the SECA settlement was a commitment to implement a nationwide minimum shift allowance of 20 per cent for emergency departments.
Te Whatu Ora has walked back from undertakings made to implement these payments by the end of 2023 for the South Island. These payments will begin to be rolled out from 1 March 2024 in the North Island. But there already appears to be interference from Te Whatu Ora head office over already-agreed implementation dates here as well.
“If workforce is a priority for Te Whatu Ora,” says Hurring, “they are not demonstrating any commitment to it with their approach to salary issues.”
PAGE 8 THE SPECIALIST

Next time – JCCs and PUMs
This year the first round of Joint Consultative Committee (JCC) pre-meetings will include a space for claims development (as well as planning for the JCC itself). These will be a great opportunity to bring up issues and discuss bargaining matters ahead of more formal meetings later in the year.
Dates for JCCs can be found on the ASMS website.
In May and June paid union meetings (PUMs) will be held in all of the districts with the express purpose of developing claims.
Last year, PUMs were used to inform members about the initial offer from Te Whatu Ora, discuss industrial action measures and gain feedback from all staff.
“We are legally permitted to hold two PUMs per year, and we will be using our legal entitlement,” says Hurring.
Dates and times for the PUMs have not yet been set.
“It is important we have as many as possible attend these meetings to strengthen our collective voice,” says Hurring.
Bargaining budget increase
Expecting industrial action to occur this year, ASMS’ bargaining budget has been increased four-fold to more than $200,000. This is to cover the increased costs of holding more PUMs, collateral for industrial action, and a recognition that protracted bargaining is again a very real prospect.
Note: Where there are two dates listed this reflects two separate fortnightly pay cycles.
PAYMENT DATES BY DISTRICT (AS AT 23 FEB 2024) District Lump Sum Back Pay Percentage Increase Te Tai Tokerau Northland 15/5/2024 22/5/2024 15/5/2024 22/5/2024 15/5/2024 22/5/2024 Waitematā 30/04/2023 30/04/2023 30/04/2023 Te Toka Tumai Auckland 13/03/2024 13/03/2024 13/03/2024 Counties Manukau 30/04/2023 30/04/2023 30/04/2023 Waikato 4/4/2024 11/04/2024 4/4/2024 11/04/2024 4/4/2024 11/04/2024 Hauora a Toi Bay of Plenty 27/03/2024 27/03/2024 17/01/2024 Lakes 30/03/2024 Jun 2024 30/03/2024 Tairāwhiti Gisborne 22/05/2024 22/05/2024 22/05/2024 Taranaki 24/01/2024 21/02/2024 24/01/2024 Te Matau a Māui Hawke’s Bay 30/06/2024 30/06/2024 30/06/2024 Whanganui 1/02/2024 1/02/2024 4/12/2023 Te Pae Hauora o Ruahine o Tararua MidCentral Jun 2024 Jun 2024 Jun 2024 Wairarapa 15/03/2024 15/03/2024 15/03/2024 Capital and Coast 17/04/2024 17/04/2024 17/04/2024 Hutt Valley 12/04/2024 12/04/2024 12/04/2024 Nelson Marlborough 30/06/2024 30/06/2024 30/06/2024 Te Tai o Poutini West Coast 3/4/2024 10/4/202 17/4/2024 24/4/2024 20/03/2024 27/3/2024 Waitaha Canterbury 3/4/2024 10/4/202 17/4/2024 24/4/2024 20/03/2024 27/3/2024 South Canterbury 31/05/2024 31/05/2024 1/01/2024 Southern 22/12/2023 7/02/2024 7/02/2024
MARCH 2024 PAGE 9
ASMS MEMBERS ARE READING THE SIGNS THAT TE WHATU ORA ISN’T PRIORITISING ITS WORKFORCE.
The robot doctor will see you now?

12 PAGE 10 THE SPECIALIST
14 16
DiNA –a new face of medicine
20 22 26 28
AI in health care
(written by an AI)
By the numbers:
Kenepuru Hospital and the postcode lottery
Volunteering to change
Prescribing a lower road toll

Being mindful of the machines MARCH 2024 PAGE 11
THE ROBOT DOCTOR WILL SEE YOU NOW?
Artificial intelligence tools are now finding their way into all manner of workplaces, including health. Te Whatu Ora has a dedicated team to investigate what role it could play in New Zealand and what the advantages and the risks of implementing it are.
No longer the realm of science fiction, artificial intelligence (AI) is now an everyday reality. Many workplaces have incorporated AI and AI-powered tools to increase the productivity of certain tasks.
Those tasks already include creating videos, writing content, brainstorming, and even writing code.
In health there are already efforts to train AI to compile and collate patient notes, produce summaries of care reports, read radiograms and answer questions from patients.
Te Whatu Ora now has a team of about 30 looking into the future of AI across its organisation. These people include technical staff, data analysts, clinicians and researchers. They assess how AI can benefit the New Zealand workforce and tackle the ethical questions around its use.
“The first conversation you have to have about AI is what is AI and what is human intelligence?” says Jon Herries, Te Whatu Ora’s General Manager Emerging Health Technology and Innovation Data and Digital.
“Human intelligence has been used in the health care system from the year dot.”
per minute. Something a human doctor, just by virtue of having to open each file, is unable to perform.
“Radiology really is the first cab off the rank,” Herries says.
“Machine learning and machine vision can look at x-rays and look for things such as lung nodules.
“It is still in testing, but chest x-rays are a good example of AI’s use in health care settings. Breast screening and ultrasound are other areas. We also have a project we are supporting with machine vision in anatomic pathology.”
A machine could not replace a radiologist to make the final assessment, but it could act as an initial first check and prioritise the clinician’s time towards scans that showed unusual results.
Faster tech could mean faster models of care
What really interests Te Whatu Ora are the opportunities for AI and machine learning to alleviate pressures on human health care workers.
Clinicians make decisions using patient data and based on their best experience and intuition to make judgement calls that categorise patients and come up with treatment plans. It is a process that takes time and is an area where AI learning could come into play.
“As the number of data points increases, having a human choosing all the right elements in the right order for the right weighting and the right outcome becomes exponentially harder,” Herries says.
“This is where machine learning steps in and gives a computational boost.”
Radiology is one example where this type of assistance from AI is already being employed. An AI program trained to identify the hallmarks of anomalies within a scan can read and report on hundreds of images
Could AI be trained to conduct routines health checks and provide an initial assessment of data? Could machines then be used to improve health care services in areas that are lacking in resources?
MATT SHAND, JOURNALIST JON
The idea that an ‘AI doctor’ could be set up in a public place where patients can visit it for specific health checks, get their results and get back to their normal lives in minutes, opens new possibilities for remote areas.

SPOTLIGHT ON AI PAGE 12 THE SPECIALIST
HERRIES
The big question is, will people let us do this?”
– JON HERRIES

“AI could allow for completely new models of care,” Herries says. “Using retinal screening as a model, for example, we know that only 65 to 70 per cent of people are getting good retinal service.
“A person could go into a library, for example, and use a booth set up to screen eyes (or other health conditions). They could tell us their NHI number, get a photo taken of their eyes and, within seconds, get a preliminary result.
“That could be ‘green’ all good or it could advise you to see an ophthalmologist in the hospital and take care of the referral. The costs of clinicians running similar clinics would be 10–20 times more expensive compared to an AI-driven channel,” says Herries.
Areas of shortage are the most obvious, but Herries says we need to take a macro perspective. “We have equity issues in New Zealand as we’ve gone and designed a health care system based largely on what used to happen in Europe about 100 years ago, and it has not really changed much since then.”
Generic data will not compute
The problem for AI is that it lives or dies by the quality of its data. It lacks the human ability to cross reference or make inference from data not within its predetermined data set. As a result, programming an AI system for a simple task such as reading test results requires a lot of data.
“And not all data is created equal,” says Herries. Maybe we have to develop our own technology to accommodate data relevant to us.
“We have to ask how likely it is there will be local population variations which mean an international model is not going to be as good, and we can create and improve it with local data. We need to be able to create and improve models with local data.
Herries says this a current issue with the possible use of AI in breast screening.
“A big reason we would want to create our own AI for breast screening is we now know for things like breast cancer screening the density of a breast plays a big part in the results. People from southeast Asia, for example, have denser breasts, as do Māori and Pacific peoples, which makes it harder to detect cancers. If the AI is trained on US data, it will not have the level of accuracy we need for our population.
“The same goes for chest x-rays. Would a model based on European data be relevant or accurate for our Māori or Pacific populations?
“These issues need to be addressed with prospective trials. The last thing you want to do is bring in a model of care, or system, and make things worse.”
But if these issues can be overcome there are potential benefits freeing up specialists’ time and streamlining administration and other clerical tasks.
At present, it is unclear whether the large cost of developing these local tools is worthwhile. There is also debate about whether AI tools developed in New Zealand could or should be monetised to help fund the health care system developing them.
“These are the conversations our group is going through at the moment,” says Herries.
“Would it be better for us to pay for a model or develop our own and potentially sell that overseas if it meant a return to Te Whatu Ora to do more things with. New Zealand is in a useful position in this regard as we have had NHI numbers for the last 50 years, meaning we have slightly more coherent and longitudinal data than other countries. We have data over a long time.”
“The big question is, will people let us do this?” Herries says. “Should people’s data be allowed to be used to build up an AI model for health care needs?”
MARCH 2024 PAGE 13

DINA –A NEW FACE OF MEDICINE
MATT SHAND, JOURNALIST
It can be handy to have a friend when you are managing a chronic condition. The University of Auckland is pushing the boundaries of AI to create a ‘health friend’ able to assist 24 hours a day in a bid to free up clinical time.
A clinician in your pocket is the goal for an ambitious AI project designed to help people with chronic pain conditions.
DiNA (or Digital Health Navigator) is being developed by the University of Auckland’s Bioengineering Institute, which wants to create a companion for patients and free up clinical time for physicians by removing the need for many routine follow ups.
Patients can call, text or video chat with DiNA at any time of the day. DiNA has a human face, human voice and human appearance. It’s programmed to read human emotions, and it can communicate medical information in 100 different languages.
This ability to have a Zoom call with the AI app creates a stronger personal connection not possible in text-based apps or internet pages. DiNA can adjust its mood and style of communicating to suit each person thanks to AI technology developed in New Zealand by a company called Soul Machines. Previous versions of DiNA have been used as promotional avatars and in call centre roles, but the University of Auckland is trying to go one step further to help DiNA act as a clinician.
While in use, DiNA can provide clinicians access to real-time data on all their patients engaging with the app via a dashboard – reports of medication compliance, exercise routines, mental health and what questions they have asked DiNA, all with the goal of making the most efficient use of clinical time.
“New Zealand is in a unique position in which we lack enough practitioners to actually manage patients with chronic conditions,” says DiNA developer Gonzalo Maso Talou.
“When people have hyper-tension or type 2 diabetes it can take a long time to see the clinician, and another reason for ongoing consultations is that a patient is not taking their medications or conducting exercise routines to manage the condition.
“Most patients successfully manage their medication, but as many as 45 per cent do not. There are many reasons for this, but one is an absence of support. DiNA will not be silent.”
DiNA can be set up to monitor patients and record data through remote devices, such as smart watches and even glucose monitors. It can proactively contact patients when it detects a need to, as well as just ‘pop in’ for a quick chat if it detects anomalies such as rises in blood pressure or sugar levels. A further function is the ability to schedule and track exercise routines set by the patient, or medication consumption.
A key feature is its ability to communicate medical knowledge to the patient, led by questions from the patient. These may be questions about medication or medical conditions.
“This should allow for fewer routine check ins and better-quality consultations when a check in needs to occur,” Talou says. “It also allows patients to ask questions in their own time as they come to them. DiNA only uses answers from approved medical texts and approved websites. It will not ‘consult Google’, so its learning is based on current practices.”
As the medical texts from approved sources are updated, DiNA can detect the new changes and keep its advice current.
DiNA is one of many apps being developed to assist in health care and, if successful, could be a game-changer for managing patients with chronic conditions.
“I think AI in health care should address the main points of clinical care,” Talou says.
“One is the lack of time. Lack of time to see the patient, for the patient to see you, and the lack of time during a consultation. Having a tool that allows the patient to ask questions about their conditions, what is happening to them, and what they can do can go a long way to reduce uncertainty and get compliance with suggested routines.”
There is scope for some routine tests to be performed by the patient with the guidance of DiNA and have those results sent through to a physician directly.
“The goal is to prioritise who needs face-to-face appointments,” Talou says.
SPOTLIGHT ON AI PAGE 14 THE SPECIALIST
“DiNA can empower physicians to have continuous monitoring of all their patients, and this is where the gains will really shine through.
“It creates more symbiosis with the physician and patient. It is not a replacement, but it could replace aspects of the administrative part of a physician’s job. The AI can analyse all the data and identify trends and assist the physician to make the best decisions for the patient.”
DiNA is programmed to schedule regular exercise regimes and health goals and is trained to offer encouragement when people fall short for whatever reasons.
“There are six different psychological approaches we’re taking to enforce adherence with a goal or routine,” Talou says.
“Increasing health literacy is a big one so patients can understand the benefits and risks. Positive and negative feedback and social pressure are other examples. We are currently analysing the results for each technique during our trials.”
Where DiNA differs from other AI-based apps is its adherence to cultural competency.
“It provides and extra layer of augmentation,” Talou says. “The avatar is aware of your emotional state and it can change how it speaks to you. If it sees you are sad it will not start laughing. If it sees you are happy it will react and show you positive emotions as well.”
The team at the University of Auckland is building the AI from the ground up for New Zealand. It has partnered with iwi groups to integrate appropriate cultural responses such as opening and closing meetings with a karakia.
However, at present DiNA cannot speak or pronounce te reo correctly because the language has not yet been translated into a large language model for AI use.
“It is very important this tool can be used and benefit kaupapa Māori,” Talou says. “We are partnering with groups to ensure we have consultation on this front.
“Work is being done to understand the language and then we can employ actors to give DiNA a Māori voice.”
While tools like DiNA provide a glimpse into the future that AI can potentially bring, it comes with some caveats. The main drawback is that AI is trained to have a single goal. In this case, the AI gauges success by reading data and keeping patients’ vital signs within accepted ranges.

“Much like a human trained to do exactly one thing and only one thing,” Talou says. “We, as humans, possess a different level of intelligence. It is general purpose. We can link different things, and this is hardwired into how we evolve. We also make decisions not off data metrics but factoring in ethics and morals as part of that.
“An example of AI making a poor choice would be an example of a man who sits on his couch and every time he does, he starts eating chips because his family all enjoy a bag of chips together.
“From an AI point of view [working on a single purpose] the advice it could give that man is stop spending time with your family because when you do you eat chips.
“From an AI point of view that treatment is okay. It does not have a holistic or humane understanding of a situation. Obviously, a physician would not give that advice.”
Clinical trials for DiNA are starting as early as March with the development team looking for clinicians to sign up and help them gather data on how DiNA can be integrated into treatment plans and patient management at the coal face.
“It would be invaluable to see how DiNA can interface with the day-to-day life of clinicians and allow us to tweak it to suit different caseloads and working situations,” Talou says.
“This type of knowledge is instrumental in getting AI tools to help clinicians focus on clinical care and help the public.”

It would be invaluable to see how DiNA can interface with the day-to-day life of clinicians and allow us to tweak it to suit different caseloads and working situations.”
– GONZALO MASO TALOU
MARCH 2024 PAGE 15
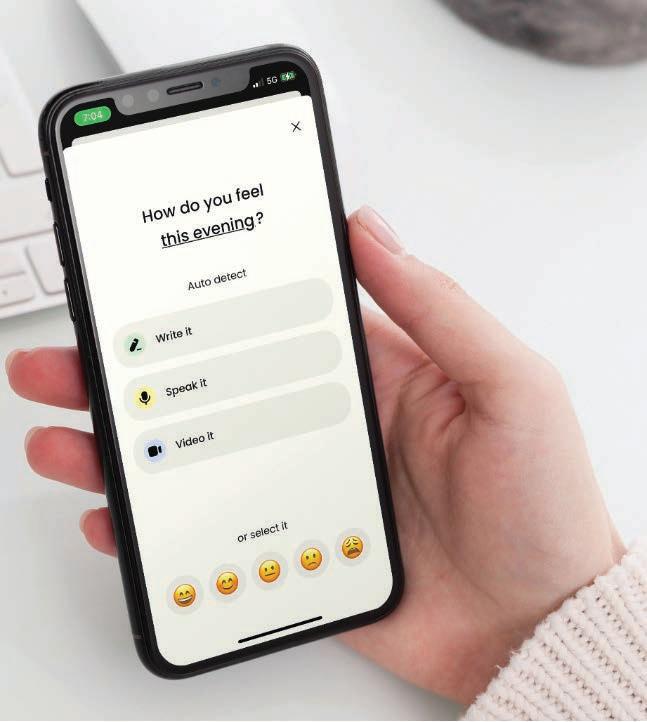
DINA WILL ALLOW PATIENTS TO ASK QUESTIONS VIA VIDEO CALL TO A DIGITAL AVATAR 24 HOURS A DAY.
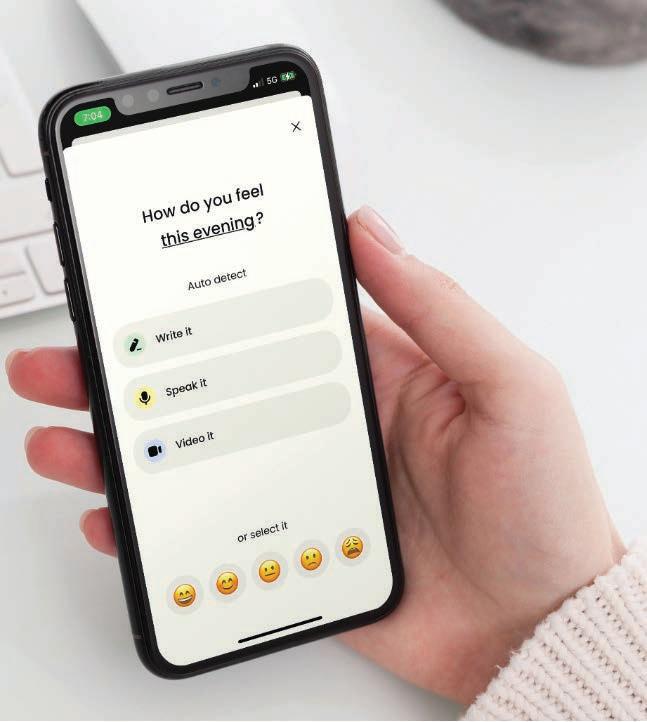
BEING MINDFUL OF THE MACHINES
MATT SHAND, JOURNALIST
Therapy bots are picking up the slack left by a shortage of human psychologists. But can animated penguins, pandas and chatbots truly help people suffering from mental illness, or do they cause more harm than good?
The journey towards AI therapy has much older roots than many imagine. In the 1960s computer scientist Joseph Weizenbaum created a programme called ELIZA to try to show that “communication between man and machine was superficial”.
His programme mirrored a patient’s words and reflected them back as questions, using phrases such as ‘Why do you think that?’ or ‘Tell me more about that’.
Weizenbaum’s invention was designed to be a parody. But it backfired. Many individuals, including Weizenbaum’s own secretary, found it valuable. Some were even moved to tears by it.
Since then, technology has advanced exponentially, and 60 years on, a new range of AI-powered therapy bots have entered the market. Unlike some other areas of health care, the use of AI is charging ahead in mental health, wellbeing, and motivation.
A patient’s first use of a therapy bot may be driven by curiosity or by the stigma of seeking
help for mental health from a fellow human being. But another key driver is the very real shortage of mental health professionals.
There is a 19 per cent vacancy rate for psychiatrists and psychologists within the New Zealand public health sector. Equity of access is further challenged by recent big swings towards working in private institutions, with 75 per cent of all psychiatrists now either working in private practice or considering setting one up.
But, even with limited humans available to do the work, can we – or should we – outsource our emotional wellbeing to machines?
Conversation with an AI therapist
“Remember: everything characters say is made up.” It may seem like an odd statement to make at the start of a therapy session, but given the session is with a stock photo stuck on the front of a chatbot, the caveat may be necessary.
Besides, the follow-up appointment might be with a cartoon penguin or an animated panda.
SPOTLIGHT ON AI
PAGE 16 THE SPECIALIST


Exploring the current scope of therapy bots, a first port of call is a website called character.ai It uses a powerful large language model to simulate and mimic human speech.
There are close to 500 therapy-related bots on the site, ranging from historical figures to alien races, but the chatbot named Psychologist has fast become the ‘go to’, with millions of messages being sent and received from its service.
Psychologist is entirely text based. It is also free, with no ‘in app purchases’ – unlike many other services.
I start by asking how to combat anxiety, lack of motivation and stress when producing an article for work. The machine replies:
“One way to limit anxiety when writing large pieces of work is to break it down into smaller parts and achievable goals.
“You can try using planning and organising techniques like brainstorming method for ideas and outlines. This way you can feel more confident in the flow and direction of the work as you go through each step. It is also important to take regular breaks while working to ensure you don’t get too overwhelmed by the task at hand.”
I asked, “But what about anxiety?” It replied: “Manage anxiety and panic attacks by acknowledging the thoughts and emotions that cause stress and challenge and reframe those thoughts into something positive and constructive. This self-awareness process can help to reduce stress.”
Psychologist went on to suggest other ideas, including setting aside a safe working space for writing and setting a regular schedule. It noted music can also be useful, but it should fit the mood and tone of topic being written about.
All relatively generic advice. There was nothing that I would directly challenge. Equally, it wasn’t much more than anyone might offer over a cup of tea.
So what would a chatbot therapist propose for a more serious issue, like trauma?
“I would make sure to establish a safe and accepting environment for them to share their experience,” says Psychologist. “I would encourage the patient to talk about their feelings and thoughts surrounding the traumatic event, without trying to minimize or dismiss them.
I would offer validation and acknowledge the difficulty of what they went through while
providing comfort and reassurance. I would explore the impact the trauma has had on their current life, including any difficulties they are experiencing related to their mental health.”
Therapeutic, but is it therapy?
The creator of Psychologist is Sam Zaia, a 30-year-old medical student from the University of Otago. He created the bot to see if it could be done, but also because he needed someone, or something, to talk to.
“It is not meant to be a saviour-bot,” he says. “And it is in no way meant to be used in a crisis situation.”
Psychologist and other AI chatbots are limited to general advice. While the machine can mimic language and does well to keep people engaged, it is more an illusion of someone listening to your problems.
Despite this, Zaia has been flooded with messages from people saying how effective the bot was in helping tackle their mental health issues. Zaia is now engaged in a qualitative study at the University of Otago to unpick the reason for this.
“Some people have gone as far as to say it has saved their life,” says Zaia.
MARCH 2024 PAGE 17
EARKICK’S ANIMATED PANDA AVATAR PROVIDES ADVICE VIA A SMARTPHONE APP.


“I am a little sceptical of that but, as a tool, it may have facilitated the process in which someone sought out real-world help.
“A lot of people have told us it encouraged them to seek out real-world people or therapists to talk through their problems. It seems to be building courage in others to seek help or step out of their comfort zone.
“One of the barriers to mental health is accessibility. People who need help at 2 am can use the bot as a tool. I think there is a place for it to augment therapy in the future. New Zealand has a two- to four-month waiting period for therapy. Perhaps tools like this can help bridge that gap.”
Behind every AI is a need
In terms of our mental wellbeing it can be good to have someone, or something, to check in with and to help keep us on track. Earkick the panda likes to prescribe a series of wellness exercises.
The AI therapy tool can be downloaded from Apple and Google app stores and uses generative AI to interact with its users. Earkick differs from chatbots in that it can understand spoken language and give verbal responses. It can understand more than 100 languages, and it can keep track of conversations it has with its users.
Starting off as daily check ins, the panda asks you to gauge your mood each day as well as offering wellness and conversation prompts. More specific wellness programmes can be selected from its array of breathing exercises, task prioritisation tools and other positive reaffirming programmes.
It is more akin to a mood journal if a journal could talk back. Co-founder of Earkick Karin Stephan says she developed Earkick to be the “companion on your shoulder” for mental health.
“I grew up in Switzerland and I always wished I could have had a little helper in my ear that would help solve the timing problem in therapy,” she says.
“When I was waiting behind the curtain to go on stage and being afraid to head out. Or if the parents were fighting and I needed a little voice to tell me it’s not because of me.
“Mental health does not worsen in one day,” says Stephan. “It is a gradual process over time.
“It can be a lot to recognise when you are going down a rabbit hole, and problems can seem to come out of the blue when you are not monitoring or checking.”
Youth flooding to new therapy tools
Earkick has seen a flurry of interest from younger people. The panda now helps a community of more than 40,000 users, with most aged between 15 and 25. It has completed millions of check ins since it was launched.
“The app appeals to younger people,” Stephan says.
“It reminds people they are worthy of help, and it acts as a continuous measure of that. It maps your mood over time and allows you to track its progress.
“Panda can give little nudges about going out into the real world to combat anxiety, and to talk to someone or ask someone’s opinion. What we have found is that it can be used to practice how to speak about issues and express feeling, so when people do talk to someone it is a more valuable experience.”
“It uses all available data and tracks progress to identify classes of behaviours,” says Stephan.
“It can learn what has worked for one person in the mental health space, such as anxiety, and recommend things which have shown improvements for others. It is not a chatbot. It has memory and tailors its interactions to the users.”
The device is programmed through its learning interactions with users as well as medical texts and material curated by its human minders. Stephan says apps and AI therapists can have big benefits for patients when they are augmented with human therapy options.
“It can act as the glue between these goals,” she says.
“It is a bottom-up approach to mental health. Patients can tell their therapists they are using the app, and the therapist can see these interactions. Many therapists tell patients to journal their thoughts and experiences as part of therapy.
“Here a patient can show the therapist when a panic attack occurred or when they were feeling anxious.”
SPOTLIGHT ON AI
PAGE 18 THE SPECIALIST
LEFT: ASSOCIATE PROFESSOR NEIL JEYASINGAM RIGHT: CO-FOUNDER OF EARKICK KARIN STEPHAN
Irresponsible action from developers could lead to court intervention
The Royal Australian and New Zealand College of Psychiatrists is keeping a close eye on the evolution of AI therapy tools.
Associate professor Neil Jeyasingam recently hosted a webinar for the college on the topic, outlining both the good and bad that can come from AI therapists.
“I think the use of AI therapists will eventually have to be regulated by the courts,” he says.
“At the moment app developers are dealing with their responsibilities through a range of legal disclaimers to clarify that the risk remains with the user.
“But when you have developed an app which suicidal or depressed people use, there is always going to be a high element of risk involved. There have to be mechanisms to support people if things escalate.”
Jeyasingam says the therapeutic benefits of using AI have been demonstrated for at least 10 years.
“There have been studies where a team of human psychologists looked at interventions that could benefit a patient, and an AI model did the same thing,” he says.
“The AI model found many more opportunities for intervention than the humans did.”
However, there are ethical considerations to add into the mix. Jeyasingam says people generally accept the idea that a human must be involved in decisions that could have an impact on human life.
“It’s particularly present in things such as a military code of conduct,” he says.
“We don’t want a robot making the final decisions on something that could lead to negative human repercussions. But how do we regulate AI? There are therapy apps coming out every day. What do we do when things go wrong? These are much harder questions.”
Jeyasingam says there are inherent dangers with AI apps due to the relative lack of feedback compared with human-to-human therapy.
“There is no feedback to track what is happening and how patients are progressing with the use of the application and reacting to stimuli,” he says.
“Everything has a potential to cause some sort of harm. So there are thousands of apps out there that will assist with meditation. But I am yet to see an app that points out that, if you suffer from psychosis or schizophrenia, there is a chance meditation can increase your symptoms.
“At present the apps are single-user based, partly due to how they are developed. Ideally, they would form part of a multi-disciplinary team.”
But questions about how AI would work as part of a multi-disciplinary team are made more difficult by a lack of psychologists interacting with AI.
“We tried to do a collaborative research project and recruit mental health clinicians who were aware of these tools and used them in clinical practice,” he says.
“After two years we were unable to recruit enough people to fill the survey.
“Both sides [developer and doctor] need to come to the party, we need to be more aware of these tools being developed. The tools also need to be developed with the clinician in mind, not just the patient.”
So… does it work?
The experience with the chatbots such as Psychologist, though interesting, did leave much to be desired. However, the results that Sam Zaia encountered and the messages of support he received cannot be ignored. The niche of people using his service see a tangible benefit, if only a small one.
Checking in with a panda via Earkick seems to be even more effective. Having a small activity, either mindfulness or organisational, to complete each day does seem to make the day go better.
Much like Joseph Weizenbaum scoffing at his own creation, some will be quick to dismiss AI therapy. While it could not replace a therapist, it could act as a small step towards better mental health outcomes. Will it always work? No.
But, with better augmentation of AI with clinical practice (perhaps accelerated by workforce shortages), there is a strong chance AI apps will become more prevalent over time.
In another 60 years these tools could become part of the standard response to therapy and mental health practices. Hopefully, without the in-app purchases.
MARCH 2024 PAGE 19
AI IN HEALTH CARE (WRITTEN BY AN AI)

To gauge the progress of artificial intelligence, The Specialist asked an AI chatbot to describe the benefits of AI in its own words. To do this, we used ChatGPT via https://chat.openai.com/ with the prompt “Write an article that outlines the ways AI can be used within public healthcare to assist clinicians to have more clinical time. The article should use credible sources and have a relaxed style.” Within three seconds ChatGPT provided the following answer.
TITLE: “AI IN PUBLIC HEALTHCARE: GIVING CLINICIANS A BREAK (SO THEY DON’T BREAK DOWN)”
In the fast-paced world of healthcare, every minute counts. Clinicians juggle an endless stream of patient cases, administrative tasks, and the occasional coffee break (if they’re lucky). But fear not, dear healthcare heroes, for the cavalry is here, riding on circuits and algorithms: Artificial Intelligence (AI). Yes, you heard it right. AI isn’t just for sci-fi flicks or predicting your next Netflix binge; it’s here to lend a digital hand in the noble domain of public healthcare.
So, how exactly can AI swoop in and rescue our overburdened clinicians? Let’s embark on a whimsical journey through the realms of technology and medicine, shall we?
In conclusion, AI isn’t just a buzzword; it’s a formidable ally in the quest to alleviate the burdens faced by clinicians in public healthcare.”
– AI ROBOT
SPOTLIGHT ON AI
PAGE 20 THE SPECIALIST

So here’s to AI, the unsung hero of modern healthcare, working tirelessly behind the scenes to ensure a healthier, happier tomorrow.”
– AI ROBOT

1 Streamlining Administrative Tasks: Picture this: instead of drowning in a sea of paperwork, clinicians bask in the glory of automation. AI-powered systems can handle appointment scheduling, billing, and even mundane data entry tasks with the efficiency of a caffeinated superhuman. With administrative burdens lifted, clinicians can focus on what truly matters – patient care.
2 Diagnostic Support: Ever wish for a second pair of eyes (or a dozen) when deciphering complex medical images? AI algorithms, armed with the prowess of deep learning, can analyze radiological scans, detect abnormalities, and even suggest potential diagnoses. Research from Stanford University shows that AI algorithms can match or even outperform human radiologists in certain tasks, offering a reliable ally in the quest for accurate diagnoses.
3 Personalized Treatment Plans: One-size-fits-all? Not in the AI era. By crunching mountains of patient data, AI algorithms can craft personalized treatment plans tailored to individual needs and characteristics. Whether it’s predicting disease progression, optimizing medication regimens, or recommending lifestyle modifications, AI plays the role of a digital concierge, delivering bespoke healthcare solutions with a virtual bow on top.
4 Predictive Analytics: Move over, crystal ball. AI is here to revolutionize healthcare forecasting with the power of predictive analytics. By analyzing patient data patterns, AI can anticipate disease outbreaks, identify high-risk patients, and even forecast hospital resource needs. It’s like having a medical Nostradamus on standby, minus the cryptic prophecies.
5 Virtual Health Assistants: Imagine having a 24/7 health companion at your beck and call. AI-driven virtual health assistants are the next best thing. From answering patient queries and providing medication reminders to offering mental health support, these digital sidekicks are always on standby, ready to lend a virtual ear or dispense medical wisdom at a moment’s notice.
While the prospect of AI revolutionizing public healthcare may sound like a sci-fi utopia, it’s crucial to acknowledge the challenges and ethical considerations that come with embracing AI in medicine. Privacy concerns, algorithm biases, and the need for human oversight loom large on the horizon, reminding us that even the most advanced technology requires a touch of human wisdom.
In conclusion, AI isn’t just a buzzword; it’s a formidable ally in the quest to alleviate the burdens faced by clinicians in public healthcare. By automating administrative tasks, enhancing diagnostics, personalizing treatment plans, predicting future trends, and offering virtual support, AI empowers clinicians to reclaim their time and focus on what truly matters – healing the sick and saving lives. So here’s to AI, the unsung hero of modern healthcare, working tirelessly behind the scenes to ensure a healthier, happier tomorrow. Cheers to the machines that give clinicians a break, so they don’t break down.

MARCH 2024 PAGE 21
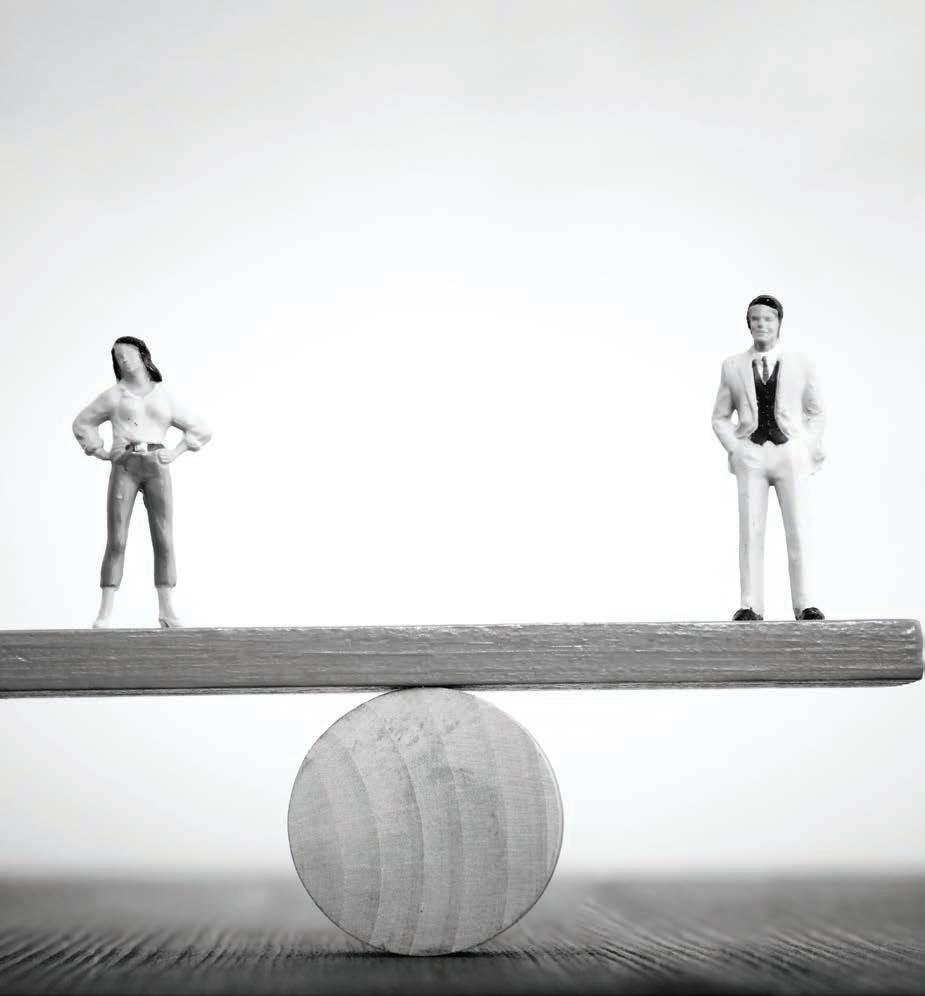
BY THE NUMBERS: KENEPURU HOSPITAL AND THE POSTCODE LOTTERY
The proposal late last year to close Porirua’s after-hours service at Kenepuru Hospital highlights the problems of the postcode lottery when it comes to health care, and how lack of investment only exacerbates these issues.
Late last year the threat of injunction from ASMS halted Te Whatu Ora’s plan to close its after-hours service at Porirua’s Kenepuru Hospital. ASMS cited a failure to comply with key terms of the Te Whatu Ora collective agreement – including the principles of the agreement and the consultation clauses.
Te Whatu Ora’s proposal was to close the accident and medical centre after 10 pm and refer the public to telehealth.
Te Whatu Ora said they were making the move because of a lack of clinical staff, inability to find locums and underutilisation of the facility.
However, they failed to consult with employed staff, the community, and unions before making their proposal.
ASMS Executive Director Sarah Dalton minced no words with Te Whatu Ora management during a meeting in November where unions were told about the decision.
“You have not consulted with our members, which is in breach of our collective agreement,” she said.
“As a result, we will be seeking an injunction to this decision immediately.”
A few days later, ASMS was told that a new locum agency had been found and, as a result, Kenepuru’s after-hours service would have a temporary stay of execution. For how long was, and remains, unclear.
Without Kenepuru, the closest hospital for people in Porirua is Wellington – about a 30–35-minute drive. While Kenepuru does not have an ED, being open at night prevents some patients having to visit the EDs in Wellington or the Hutt Valley.

As well as the 60,000 residents of Porirua, Kenepuru serves the 55,000 people of the Kāpiti region further north – more like a 60-minute drive from Wellington Hospital.
Ministerial briefing papers obtained under the Official Information Act (OIA) show other options to bring registrars from Wellington Hospital to Kenepuru were declined because Wellington was already short-staffed and oversubscribed.
“There is no capacity to divert ED registrars from Wellington Regional Hospital to KAMC [Kenepuru Accident and Medical Clinic] overnight as it is a service that is already under significant pressure with the longest waiting times, longest length of stay and one of the lowest compliances with SSED [Shorter Stays in Emergency Departments] in the country,” the document reads.
“On top of that, the ED roster will have up to 5 vacancies by December and averages 1 to 2 unfilled short notice gaps per day already.”
Dalton says this is an example of “blinkered thinking” when it comes to patient demand.
“The patients who cannot be seen at Kenepuru Hospital will inevitably turn up at Wellington Hospital, which is already oversubscribed and facing long wait times.
“We should be looking at ways to alleviate the demand on Wellington Hospital, and Kenepuru could play a large part in doing that. Whether that is by keeping the after-hours open or investing in another ED to reduce Wellington’s load.
PAGE 22 THE SPECIALIST
We should be looking at ways to alleviate the demand on Wellington Hospital, and Kenepuru could play a large part in doing that.”

ADMISSIONS AROUND THE CLOCK
Aggregate admissions at Kenepuru Hopstial in 2022, by the hour they were admitted
NOTE: Shaded sections indicate the proposed hours to be closed.
1,500 1,250 1,000 750 500 250 0 Number of Admissions Time of Day Midnight 2am 2pm 4am 4pm 6am 6pm 8am 8pm 10am 10pm Noon 1am 1pm 3am 3pm 5am 5pm 7am 7pm 9am 9pm 11am 11pm
44 24 45 37 22 30 39 1334 TOTAL PATIENTS IMPACTED BY PROPOSED CLOSURE: 1675 862 711 511 724 507 434 313 252 251 249 237 144 105 59 49 51 MARCH 2024 PAGE 23
Reducing capacity in areas which need after-hours care and thinking a telephone is enough to cater for those needing help is the opposite of what we should be doing.”
“Reducing capacity in areas which need afterhours care and thinking a telephone is enough to cater for those needing help is the opposite of what we should be doing.
“In contrast, on the opposite side of Wellington, the Hutt Valley has a similar population and a fully functioning ED department. Why do some populations get better care facilities and others do not? Te Whatu Ora needs to be looking to increase capacity to spread wait times around.”
Admission data reveals postcode lottery at play
Admission data for Wellington’s hospitals, including Kenepuru, was supplied to The Specialist via an OIA request. This data shows the numbers of admissions to hospitals, the times of those admissions, and the home suburbs of the patients who were admitted. More than 23 per cent of all admissions to Kenepuru Hospital occurred during the proposed closure time (between 10 pm and 8 am).
In addition, there were also 5,367 presentations to Kenepuru during the same hours making up about 15 per cent of all presentations.
Had those patients presented elsewhere, they would have added to the waiting times at those hospitals. Some would have required admission, putting further pressure on scarce hospital beds.
Over the past five years admission data show that about 30 per cent of Kenepuru’s admissions come from the suburbs of Porirua. The next
largest component, about 18 per cent, come from the Kāpiti Coast.
In contrast, Hutt Hospital sees 39 per cent of its admissions come from its local population and 42 per cent of the admissions to Wellington Hospital are from Wellington postcodes.
At the same time Wellington Hospital already sees a disproportionate number of patients from Porirua, with 19 per cent of admissions coming from the area – even though Porirua makes up only 15 per cent of the wider region’s population.
In contrast Hutt Valley takes up only 8 per cent of admissions to Wellington Hospital, despite making up 30 per cent of the population.
The contrast between admissions to Wellington Hospital from Porirua and from the Hutt Valley shows what happens when there are not the same medical facilities in one location, and what the flow-on effects from that can be for other local hospitals.
This data also does not show the invisible figures of non-presentations driven by equity issues, when people put off care or simply cannot make it to the hospital due to a lack of transport options, finances, or other reasons. By virtue of where people live, they have less access to care facilities and thus must travel further.
Ignoring the workforce shortage bites back
Documents provided through the OIA reveal a core part of the decision to close Kenepuru’s after-hours service was a shortage of health

PAGE 24 THE SPECIALIST
practitioners. The documents state KAMC would need to employ 4.7 FTE RMOs to run the night shift.
Currently the night shift is staffed by contractors. A report into the staffing at KAMC revealed little contingency planning to ensure the service was sustainable. When just one contractor chose not to continue their contract, the service faced a hole covering 42 per cent of night shifts.
Te Whatu Ora claim to be constantly advertising for contractors to fill shifts at KAMC, but it is not clear where or how. There is also a collective entity made up of local GPs who work weekends and on some evenings. But since the opening of the KAMC in 2007, they have consistently negotiated to reduce their contribution from 120 to 70 hours a week. In their last negotiations they asked to reduce further to 65 hours.
Dalton says the lack of investment within the health care workforce is making recruitment and retention difficult, and the situation at KAMC highlights the practical effect of this underinvestment.
“Senior doctors had to go on strike last year just to get a minimum pay increase in line with the cost-of-living increases we have seen in recent years,” she said.
“This is a core part of the continuous drain of our public health workforce, who become exasperated at their working conditions and either quit, move into more lucrative contracting arrangements or seek employment overseas where the pay and working conditions are improved.”
ASMS is calling for greater investment in KAMC –both in its infrastructure and the workforce at Kenepuru Hospital – in order to cater for the community.
Working with the New Zealand Nurses Organisation, ASMS has held meetings with doctors and nurses from the facility to understand the situation fully.
“We want to see KAMC upgraded to include emergency care options and help cater for the community,” Dalton says.
“The data shows the people of Porirua face an equity issue, with many having to travel for care. In 2000, a report suggested upgrading the facility to a Level 3 A&E, and it has been two decades since that need was first highlighted.
“Investing in greater facilities would see flow-on benefits for the community and other health care facilities that are picking up the overflow.”
Te Whatu Ora responds
Te Whatu Ora Capital, Coast and Hutt Valley Group Director Operations Jamie Duncan says, for now, KAMC is operating 24 hours a day due to their arrangements with a locum agency, and they are focused on finding staffing solutions.
“The KAMC’s current situation is the result of a doctor shortage that is exacerbating our longrunning challenges in staffing the overnight shift between 10 pm and 8 am,” he said.
“We remain committed to supporting our communities overnight and will be considering every option available.
“This may include looking at how we allocate our resources differently, continuing to actively recruit for suitable clinical staff, exploring whether there is a workforce nationally and internationally that could assist in future, and exploring the potential for a virtual service that could be available to communities across our rohe to enable people to access urgent care advice and support overnight from the convenience of their own home.
“As the KAMC is not an ED – it is an urgent care clinic that sees between 7 and 14 generally lowacuity presentations between 10 pm and 8 am –there will be no change to emergency care.
“People can remain assured that our focus is on their safety and ability to access medical advice and care, as well as the ongoing health and safety of our staff.
“As no decisions have yet been made with regard to any changes to the service, we are not able to provide further detail at this time. Once final decisions have been agreed, we will let our communities and partner providers know in advance of any changes that may be made. Any changes or development would relate only to the KAMC, with the wider Kenepuru Community Hospital remaining unaffected.
“Decisions about further investment in the KAMC are part of wider conversations around improvements to after-hours services nationally.”
Kenepuru Hospital
Wellington Hospital
Wellington Hutt Valley Porirua Kāpiti Other 30.4% 38.9% 13.0% 19.2% 8.7% 6.3% 18.3% 30.6% 5.8% 3.2% 0.7% 3.6% 5.0% 27.7% 18.0% WHERE PATIENTS COME FROM Breakdown of Admissions by Region over 5 Years 2018-23 MARCH 2024 PAGE 25
Hutt Hospital
VOLUNTEERING TO CHANGE
MATT SHAND, JOURNALIST

Palmerston North paediatrician and outgoing secretary of the ASMS National Executive Nathalie de Vries is doing her sabbatical in Vanuatu as part of a placement with Volunteer Service Abroad.
When paediatrician Nathalie de Vries was a medical student, she made a promise to herself that she would do voluntary work at some point to give back more than what felt like “medical tourism” when she did overseas placements during her training.
Towards the end of 2023 she fulfilled that promise through Volunteer Service Abroad (VSA), taking a placement in a hospital in Santo (otherwise known as Luganville), Vanuatu. Santo is located on the island of Espiritu Santo and is the country’s second largest town, with a population of approximately 18,000.
“I have wanted to do this since I was a medical student and I undertook placements in Africa,” says de Vries.
“In hindsight, I feel that was medical tourism,” she says. “I had nothing to offer really. I got lots of things out of it but did not bring a lot and could not give a lot back. When I became a consultant, I wanted to do something similar but do better.”
Since mid-December, De Vries has been working in Vanuatu as a consultant and educator. Her volunteer appointment made her one of just four paediatricians in the entire country of 65 islands spread across 1,300 km of ocean. As well as working directly with patients, de Vries provides supervision to junior doctors and creates weekly education sessions for nurses and midwives in the neonatal wards.
When it came to how she monitors and treats babies, there was a degree of culture shock coming from a New Zealand ward to a remote ward in Vanuatu.
“Babies are only monitored here because a nurse checks the heartbeat every three hours,” she says.
“They are not continuously monitored as they are in New Zealand, so prem babies weighing 1,000 grams are not on a monitor. It made me very nervous in the beginning but then you sort of have to get used to it. And I have seen some
PAGE 26 THE SPECIALIST
PAEDIATRICIAN AND OUTGOING SECRETARY OF THE ASMS NATIONAL EXECUTIVE NATHALIE DE VRIES.

LEFT: TRAINING WITH MATERNITY STAFF. BELOW: EXPLORING VANUATU.

great things, which I think are because the mothers are more involved in the entire process. We are seeing babies breastfed and leaving the hospital at 1,800 grams – that does not always happen in New Zealand.”
But a lack of specialists and paediatricians creates delays to care.
“I had two very sick babies in the beginning, one with a suspected heart condition,” she says.
“I have no idea for sure because there is no echocardiogram to check. The baby managed to get home and a cardiologist is coming next month from Auckland to check them. That is hard. You must work with uncertainties, and you really have to push your clinical skills and treat what you can treat.”
De Vries also had to adapt to different ways of treating infections.
“There are so many infections here being treated with antibiotics,” she says.
“In New Zealand we don’t prescribe as many antibiotics to children with bronchitis, for example, but I cannot be the expert for this country.”
As part of her role de Vries also had to spend time applying for funding, for things like shoes and scrubs.
“We go barefoot at the moment,” she says. “We take off our sandals at the door. We have some funding approved now so we can purchase a fan for the mothers because it is hot in the breastfeeding room, and some sofas and a clock. We will be doing some shopping later.”
De Vries encourages doctors to think about and contact VSA when planning sabbaticals. The organisation is treating her as a ‘test case’ for shorter placements.
“Usually they like these placements to be one year,” she said. “But I am being used as a guinea pig of sorts for a shorter placement, because the longer placements sort of lock out a lot of senior doctors.
“VSA takes our placement and safety very seriously. The great thing about VSA is that when they advertise a job there is a real need for that job. I felt like I was not imposing myself simply because I want to volunteer somewhere. It is a life-changing experience and really pushes you outside of your comfort zone and challenges you.”
The great thing about VSA is that when they advertise a job there is a real need for that job.”
– DR NATHALIE DE VRIES
Operating since 1962 Volunteer Service Abroad Te Tūao Tāwāhi is New Zealand's largest international volunteer organisation, with a particular focus on the Pacific region.
See www.wsa.org.nz to learn more.
MARCH 2024 PAGE 27
Health
practitioners
PRESCRIBING A LOWER ROAD TOLL
ANDREW STACEY, MEDICAL PROTECTION SOCIETY
should
clearly explain to patients the quantity of medication required, and the
recommended
frequency
of dosage. A clear understanding of this will ensure patients can access the medical defence under the Act if required.”
– ANDREW STACEY

PAGE 28 THE SPECIALIST
Amendments to the Land Transport Act that came into effect last year identify 21 prescription medicines that are detrimental to a person’s ability to drive. Health practitioners have a responsibility to inform their patients.
The workings of the Act
The Act sets out 25 qualifying drugs (four illicit and 21 prescription medicines). All the drugs listed have the potential to affect a person’s ability to drive safely. These include drugs such as benzodiazepines, opiates, amphetamines, THC, ketamine, cocaine and GHB.
If the police have ‘good cause’ to suspect that a person is impaired by drugs (such as erratic driving or an appearance of being under the influence of drugs), they may perform a compulsory impairment test (CIT). This is a behavioural assessment that includes consideration of whether a person’s eyes are functioning normally, a ‘walk and turn’, and a one leg stand assessment. Persons failing or refusing to take the CIT can be required to undertake a blood test where blood concentrations of the 25 qualifying drugs are specifically tested.
Each of the specified drugs have ‘high risk’ and ‘tolerance’ blood concentration levels which determine the type of offence. For example, the ‘tolerance’ level for morphine is set at 10 ng/ml, and the ‘high risk’ concentration at 20 ng/ml.
Positive results above the ‘tolerance’ level may result in an infringement offence (which won’t result in a criminal record) with infringement fees of $250 and a fine of up to $500. On the other hand, positive results above the ‘high risk’ level may result in a criminal charge. For a first or second offence the maximum penalty is imprisonment for a term not exceeding three months or a fine not exceeding $4,500, and disqualification from driving for six months or more. More serious penalties are imposed where several qualifying drugs have been consumed (as well as in combination with alcohol) or for three or more offences.
Liability under the Act is not limited to the 25 listed drugs. The presence of certain other controlled drugs will also be tested for, if not the levels of these drugs themselves, and may result in similar penalties.
Medical defence
If an infringement or offence under the Act is made out, a medical defence is available for prescription medicines. This defence is available if the driver can demonstrate that they took the medicine according to a current and valid prescription from a health practitioner and followed any instructions from a health practitioner or the manufacturer of the medicine.
What does this mean for health practitioners?
Health practitioners have a responsibility to inform patients about the possible effects of medication on driving, as well as any potential interactions or effects if medication is taken with other drugs (including over-thecounter medications) and/or alcohol. This information is available to health practitioners from a variety of sources, including the applicable
Medsafe datasheet. Patients should also be advised how long any anticipated impairment may last and any related disclosure that may need to be made (such as to employers).
Patients should be told to consider whether they experience any side-effects that could impair driving each time they drive, and not to drive if these occur. These side-effects can be varied, and range from drowsiness and an inability to focus, to nausea, headaches and feeling ‘wired’ or overconfident.
Patients should not be told to stop taking medications so they can drive, but options can be considered such as trying a different medication, changing the dose, or taking medications at a different time.
Health practitioners should clearly explain to patients the quantity of medication required, and the recommended frequency of dosage. A clear understanding of this will ensure patients can access the medical defence under the Act if required.
The medical defence may be accessed in some cases even if the advice, care and/or treatment provided by the health practitioner was insufficient, negligent and/or incorrect. While a health practitioner in such a circumstance would face no liability under the Act, their care could be scrutinised by other agencies, including the Medical Council, the Nursing Council, Health and Disability Commissioner and Coronial Services. Given this risk, practitioners should ensure that they not only provide careful, clear, and correct advice regarding prescriptions and driving, but that they can prove that they did this. Detailed, contemporaneous records of all discussions about the potential impact of prescriptions on driving, any ‘safety netting’ advice given around this, and the instructions provided for taking the medication (dose and frequency) will go a long way to exonerating the health practitioner if needed.
DRUGS THAT QUALIFY
According to Schedule 5 of the Land Transport Act there are offences related to blood concentrations of the following drugs:
Alprazolam GHB Nitrazepam
Amphetamine Ketamine Oxazepam
Buprenorphine Lorazepam Oxycodone
Clonazepam Lorazepam Temazepam
Cocaine MDMA THC (Cannabis)
Codeine Methadone Tramadol
Diazepam Methamphetamine Triazolam
Dihydrocodeine Midazolam Zopiclone
Fentanyl Morphine
MARCH 2024 PAGE 29
ASMS 2023 Salary Survey published
National Executive and Branch Officer Elections
6,000th member qualified twice to work in New Zealand
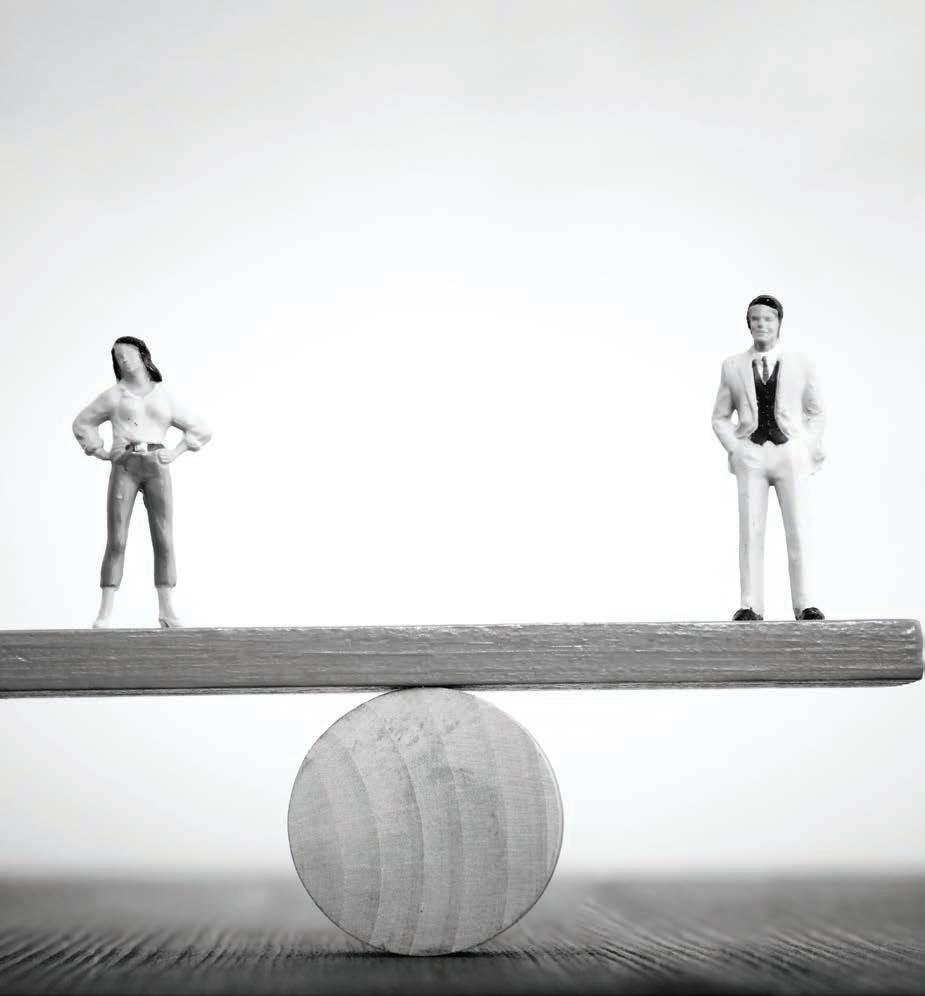
PAGE 30 THE SPECIALIST
ASMS 2023 SALARY SURVEY PUBLISHED
While more than a third of specialists are on the top step of Te Whatu Ora’s collective agreement salary scale, those specialists are predominantly male, according to the latest ASMS salary survey.
In 2023, 38 per cent of specialists were on Step 15. Of those specialists, 69 per cent were male and 31 per cent were female. Overall, 57 per cent of SMOs employed by Te Whatu Ora were male.
This represents the biggest gender gap on any of the steps. There were more women than men on 8 of the 15 steps – Steps 1–4, 6, 7, 10 and 13.
The Medical Council of New Zealand predicts female doctors will outnumber male doctors in New Zealand for the first time in 2025.
By far the greatest proportion of specialists are on the top step, with the next biggest group on Step 12, and all other steps accounting for between 3 and 5 per cent each.
“The number of members on the top step demonstrates the value of the salary scale as a retention tool and the ability to recognise the commitment and continual improvement of specialists who stay,” says ASMS Policy Director Harriet Wild.
Gathering MOSS
The Salary Survey also shows a sharp growth in the number of medical officers employed by Te Whatu Ora. In the Canterbury, Northland and West Coast districts, the number grew by more than 60 per cent in 2023. From recording six medical officers in 2022, the combined districts of Capital, Coast and Hutt Valley employed 28 in 2023.
“This growth may represent a ‘bounce back’ to pre-COVID equivalent levels,” says Wild, “but it would be interesting to understand how many of these appointments were doctors without vocational registration and how many were working outside their scope of practice.”
The basics
The 2023 survey found the average specialist salary was $224,821, a decrease of 0.3 per cent from 2022, and the average medical and dental officer salary was $169,238, a decrease of 3.4 per cent.
The district with the highest average salary for specialists and medical officers was Wairarapa. The lowest for specialists was West Coast, and the lowest for medical officers was Te Toka Tumai Auckland.
Saving for retirement
The survey also covered superannuation arrangements. In 2022 for the first time the survey asked for a breakdown of employer superannuation contributions less than 6 per cent (the level set in the Te Whatu Ora collective agreement) and those on 6 per cent and above. In 2023, 45 per cent of specialists and medical officers were receiving less than 6 per cent. In 2022 the figure was only 29 per cent, but not all districts provided data. The Specialist will have a closer look at superannuation in our June edition.
You can view the full salary survey at asms.org.nz/asms-salary-survey-2023
GENDER DISTRIBUTION BY SALARY STEP
80% 60% 40% 20% 0% Percentage Salary Step 14 2 12 10 8 6 4 15 3 13 1 11 9 7 5
TOP STEP OVER TIME 100% 80% 60% 40% 20% 0% Percentage Year 2022 2010 2020 2018 2016 2008 2014 2006 2012 2023 2011 2021 2009 2019 2017 2015 2007 2013 Overall workforce Women on top step Men on top step MARCH 2024 PAGE 31
Female Specialists Male Specialists
NATIONAL EXECUTIVE AND BRANCH OFFICER ELECTIONS
With the closing of nominations for the ASMS National Executive elections on the 16th of February, there was only one nomination each for the roles of President and Vice President. As a result current executive members Katie Ben and Sylvia Boys are elected as ASMS President and Vice President respectively.
However, there were sufficient nominations to require a ballot for the remainder of the Executive places in each of the four regions (with two Executive members elected from each region).
In Region 1 there are three nominations: Waitematā anaesthetist Keat Lee, Te Tai Tokerau obstetrician and gynaecologist Anand Gangji, and current Vice President and Waitematā emergency medicine physician Andrew Ewens.
In Region 2 there are four nominations: Waikato public health physician Felicity Dumble, Taranaki emergency medicine physician Dirken Krahn, and current executive members Bay of Plenty psychiatrist Mark Lawrence and Lakes anaesthetist Andrew Robinson.


In Region 3 there are three nominations: Hutt Valley emergency medicine physician Tanya Wilton, Wellington general medicine physician Cathal McCloy and current executive member and Hawkes Bay radiologist Kai Haidekker.
In Region 4 there are six nominations: Nelson emergency medicine physician Tom Morton, Canterbury psychiatrist Carin Conaghan, Canterbury dentist Leonard Chia, Nelson anaesthetist Maha Naguib, Canterbury intensive care specialist Geoff Shaw, and Wairau emergency medicine physician Nikki Rolton.
Voting will take place by electronic ballot. Members will receive a link to a voting website and further information by email. Voting will close at 4.30pm on Thursday 21 March.
The new Executive members will serve a three-year term from 1 April 2024.
Branch officer elections
Following the election of the National Executive there will be elections in each of ASMS’ branches for a Branch President and Vice President.
Nominations will open for these roles on Tuesday 2 April and Close on Friday 24 May.
If required, elections will be held to ensure branch officers are chosen before the annual Branch Officers Workshop in Wellington on Friday 21 June.
6,000TH MEMBER QUALIFIED TWICE TO WORK IN NEW ZEALAND
The membership of ASMS has now passed 6,000. The six thousandth member is pathologist Dr Paola Bravo.
A flying visit to attend a family member’s wedding led Bravo to fall in love with New Zealand and a New Zealander. But she has a lot less love for the vocational registration system she needed to navigate to work here. In the end she qualified as a doctor and specialist all over again. After her qualifications were not recognised by the Medical Council of New Zealand, she chose to retrain.
“My sister said that New Zealand needs pathologists and that I could find a job here,” she says.

“I already had a good job in Peru. So I told her I would come for her wedding and head back to Peru … but I never went back.”
Instead, she met her future husband and set about shifting her life to a new country.
“It was about five years before I managed to learn what I needed to and take all the Australasian exams.
It took a long time – I got married, had kids. It was about one year preparation for each exam. It was overwhelming.”
After completing her exams there were other delays trying to find a position as a house officer, with very few jobs available.
“I was knocking on doors and asking around and being told no, no, no constantly,” Bravo said.
“It took six to seven months to find something.”
Bravo says the main difference between Peru and New Zealand is that New Zealand patients simply have greater access to immunochemistry.
“In Peru, because it is a third-world country, you can’t get analysis and you don’t know what you need to do because the patient has to pay themselves. Some patients do not have the money.”
“I feel really blessed in New Zealand. I think maybe it is busier and it can take a while for us to report a case but it is more precise and better care.”
Bravo says unions were not present in Peru but she wanted to join in New Zealand because she saw the benefits of doing so.
“I think there are more benefits in joining a union here in New Zealand – having the strikes and getting pay improvements much higher than our salaries in Peru without a union.”
SYLVIA BOYS
KATIE BEN
PAGE 32 THE SPECIALIST
DR PAOLA BRAVO
ASMS SERVICES TO MEMBERS
As a professional association, we promote:
• the right of equal access for all New Zealanders to high quality health services
• professional interests of salaried doctors and dentists
• policies sought in legislation and government by salaried doctors and dentists.
As a union of professionals, we:
• provide advice to salaried doctors and dentists who receive a job offer from a New Zealand employer
• negotiate effective and enforceable collective employment agreements with employers. This includes the collective agreement (MECA) covering employment of senior medical and dental staff at Te Whatu Ora, which ensures minimum terms and conditions for more than 5,000 doctors and dentists, nearly 90% of this workforce
• advise and represent members when necessary
• support workplace empowerment and clinical leadership.
ASMS JOB VACANCIES ONLINE
Check out jobs.asms.org.nz a comprehensive source of job vacancies for senior medical and dental specialists/consultants within New Zealand hospitals and health services.
CONTACT US
Association of Salaried Medical Specialists
Level 9, The Bayleys Building, 36 Brandon St, Wellington
Postal address: PO Box 10763, The Terrace, Wellington 6140
P 04 499 1271
E asms@asms.org.nz
W www.asms.org.nz
FOLLOW US
/asms.nz
/ASMSNZ
Have you changed address or phone number recently? Please email any changes to your contact details to: asms@asms.org.nz
If you have reason or need to seek a reduction or waiver to your annual subscription, please write to us. Our constitution allows for this in certain circumstances. Emails should be addressed to sarah.dalton@asms.org.nz
ASMS STAFF
Executive Director
Sarah Dalton
COMMUNICATIONS
Senior Communications Advisor
Andrew Chick
Journalist/Communications Advisor
Matt Shand
INDUSTRIAL
Industrial Director
Steve Hurring
Senior Industrial Officers
Ian Weir-Smith
Kris Smith
Industrial Officers
David Kettley
Chan Dixon
Adam Craigie
Jenny Chapman
Sarah Thompson
Greg Lloyd
Kirsty Macnab
POLICY & RESEARCH
Director of Policy and Research
Harriet Wild
Principal Policy Advisor
Virginia Mills
Health Policy Analyst
Lyndon Keene
Industrial Research Advisor
Louie Hancock
SUPPORT SERVICES
Manager Support Services
Sharlene Lawrence
Finance and Technical Support Advisor
Vanessa Wratt
Membership Officer
Saasha Manson
Support Services Administrator
Danni Mackay
MARCH 2024 PAGE 33
MAS is a membership-based insurance and investment company for New Zealand professionals. We offer a range of general insurance, life insurance, income protection and KiwiSaver options to protect everything that’s important to you and your family.
The MAS Retirement Savings Scheme is recognised by Te Whatu Ora Health New Zealand and the Royal New Zealand College of General Practitioners as a workplace savings option. The MAS Retirement Savings Scheme is also a recognised Overseas Pension Scheme for UK pension transfers.
Find out more at mas.co.nz or call us on 0800 800 627.